Introduction to Inomyalgia
Inomyalgia is a term that has gained attention in recent years for describing a condition linked with chronic muscle pain, fatigue, and reduced quality of life. Unlike common muscle soreness, Inomyalgia involves persistent discomfort that affects daily routines and emotional well-being. Understanding its nature, causes, and management strategies is essential for individuals facing its challenges and for professionals seeking to provide better care.
Living with chronic pain can be isolating and overwhelming. Many people struggling with this condition often feel misunderstood because the pain they experience is not always visible to others. The journey toward proper diagnosis and effective management requires patience, education, and a comprehensive approach that addresses both physical and emotional aspects of health.
What Is Inomyalgia?
The condition represents a complex chronic pain disorder characterized by widespread musculoskeletal discomfort that persists over extended periods. Patients typically describe the sensation as a constant, dull ache that affects multiple areas of the body simultaneously. This pain is not localized to one specific region but rather spreads across various muscle groups, making everyday activities challenging.
Beyond physical pain, the condition impacts multiple body systems. The nervous system plays a crucial role in how pain signals are processed and perceived. Research suggests that individuals with this disorder may experience amplified pain responses, meaning their bodies interpret normal sensations as painful stimuli. This heightened sensitivity creates a cycle where even gentle touch or mild pressure can trigger significant discomfort.
The condition differs from typical muscle strain or temporary soreness that resolves with rest. While acute muscle pain usually improves within days or weeks, this chronic condition persists for months or even years. The persistent nature of symptoms significantly affects quality of life, relationships, work productivity, and mental health.
Common Symptoms and Clinical Presentation
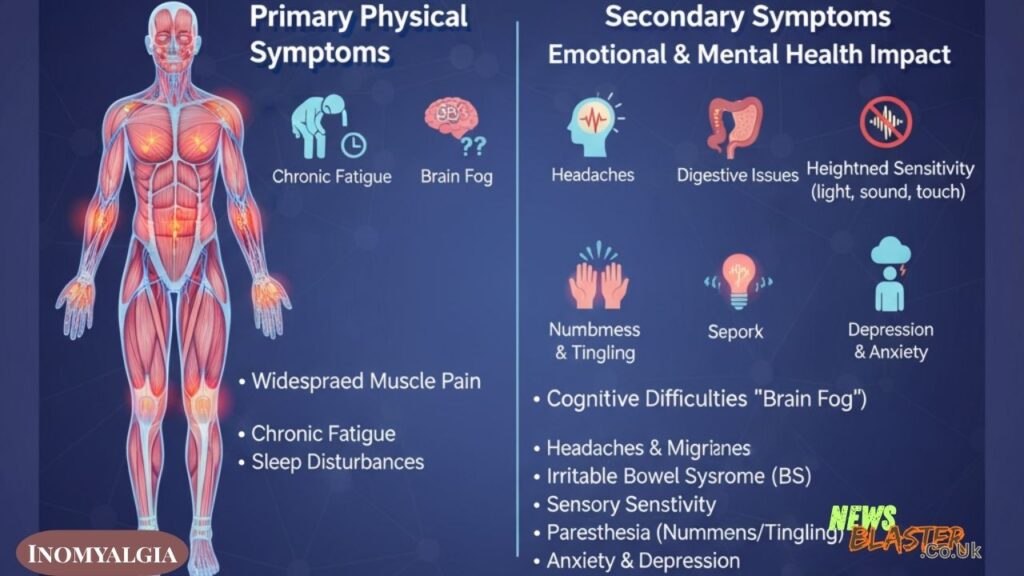
Primary Physical Symptoms
Widespread muscle pain remains the hallmark symptom that brings most patients to seek medical attention. This discomfort typically affects both sides of the body and occurs above and below the waist. The pain intensity fluctuates throughout the day, with some individuals experiencing worse symptoms in the morning upon waking, while others find their discomfort increases as the day progresses.
Chronic fatigue represents another debilitating aspect of the condition. Patients frequently report feeling exhausted even after a full night’s sleep. This exhaustion is not simply feeling tired; it is a profound sense of physical and mental depletion that does not improve with rest. The fatigue can be so severe that it interferes with concentration, decision-making, and the ability to perform routine tasks.
Sleep disturbances plague many individuals with this condition. Despite spending adequate time in bed, the quality of sleep remains poor. Many patients report waking frequently throughout the night, experiencing restless sleep, or waking up feeling as though they have not slept at all. This non-restorative sleep contributes to the ongoing fatigue and can worsen pain perception.
Secondary Symptoms
Cognitive difficulties, often described as “brain fog,” affect many patients. This mental cloudiness manifests as problems with memory, concentration, and processing information. Simple tasks that once felt automatic may require significant mental effort. Word-finding difficulties, forgetfulness, and reduced mental clarity can be frustrating and impact professional and personal life.
Headaches and migraines occur with increased frequency in individuals with this condition. These headaches range from mild tension-type discomfort to severe migraines that require rest in a dark, quiet room. The relationship between chronic pain conditions and headaches suggests shared neurological pathways and pain processing mechanisms.
Digestive issues commonly accompany the condition. Many patients report symptoms consistent with irritable bowel syndrome, including abdominal pain, bloating, constipation, or diarrhea. The connection between the gut and the nervous system, known as the gut-brain axis, may explain why digestive symptoms often coincide with pain and fatigue.
Heightened sensitivity to environmental stimuli presents another challenge. Bright lights may feel overwhelming, loud noises can be jarring, and temperature changes may trigger increased discomfort. This sensory sensitivity extends to touch as well, with some individuals finding that normal pressure or contact feels painful.
Numbness and tingling sensations in the hands, feet, arms, or legs affect many patients. These sensations, medically known as paresthesia, can range from mild pins-and-needles feelings to more pronounced numbness that interferes with grip strength and coordination.
Emotional and Mental Health Impact
Depression and anxiety frequently develop in individuals living with chronic pain conditions. The constant struggle with pain, fatigue, and functional limitations takes a toll on emotional well-being. Feelings of frustration, hopelessness, and isolation are common, particularly when symptoms persist despite treatment attempts.
The bidirectional relationship between chronic pain and mental health means that physical symptoms can worsen psychological distress, while anxiety and depression can amplify pain perception. Addressing both physical and emotional aspects becomes crucial for comprehensive care.
Understanding the Causes and Risk Factors
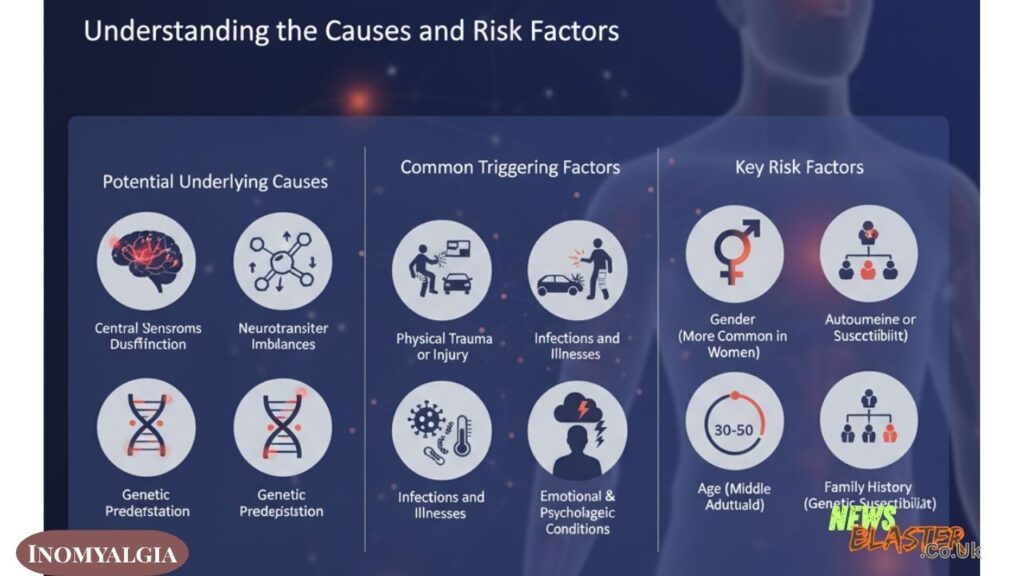
Potential Underlying Causes
The exact mechanisms that trigger this condition remain under investigation, but researchers have identified several contributing factors. Central nervous system dysfunction appears to play a significant role. The brain and spinal cord may process pain signals abnormally, amplifying normal sensations into painful experiences. This central sensitization means the nervous system becomes hyperresponsive to stimuli.
Neurotransmitter imbalances have been observed in many patients. Neurotransmitters are chemical messengers that transmit signals between nerve cells. Imbalances in serotonin, dopamine, and norepinephrine may affect pain perception, mood regulation, and sleep quality. These chemical imbalances help explain why medications that modulate neurotransmitter levels can provide symptom relief.
Genetic predisposition appears to increase susceptibility. Studies have shown that the condition tends to run in families, suggesting hereditary factors influence who develops the disorder. Having a close family member with the condition increases individual risk, though genetics alone do not guarantee someone will develop symptoms.
Common Triggering Factors
Physical trauma or injury sometimes precedes the onset of symptoms. Car accidents, falls, surgeries, or other forms of physical stress may trigger the development of chronic pain. The body’s response to trauma can potentially alter pain processing pathways, leading to persistent symptoms long after the initial injury has healed.
Infections and illnesses have been identified as potential triggers. Viral or bacterial infections may activate immune responses that contribute to the development of chronic pain symptoms. Some individuals report symptom onset following a significant illness, suggesting a possible connection between immune system activation and pain pathway alterations.
Emotional and psychological stress represents another significant trigger. Major life events, prolonged stress periods, or psychological trauma can precipitate symptom onset or worsen existing conditions. The mind-body connection plays a powerful role in how stress affects physical health and pain perception.
Pre-existing autoimmune or rheumatic conditions may increase vulnerability. Individuals with conditions such as rheumatoid arthritis or lupus show higher rates of developing chronic pain syndromes. The inflammatory processes and immune system dysregulation in these conditions may contribute to pain pathway sensitization.
Key Risk Factors
Gender plays a notable role, with women experiencing this condition at significantly higher rates than men. Hormonal differences, genetic factors, and variations in pain processing between genders may contribute to this disparity. Understanding gender-related differences helps healthcare providers tailor treatment approaches.
Age influences risk, with most diagnoses occurring during middle adulthood. While the condition can develop at any age, individuals between 30 and 50 years old represent the most commonly affected age group. However, younger and older individuals can also develop symptoms.
Family history serves as an important risk indicator. Having blood relatives with chronic pain conditions increases personal risk. This familial clustering suggests both genetic susceptibility and potentially shared environmental factors contribute to condition development.
Diagnosis and Medical Evaluation
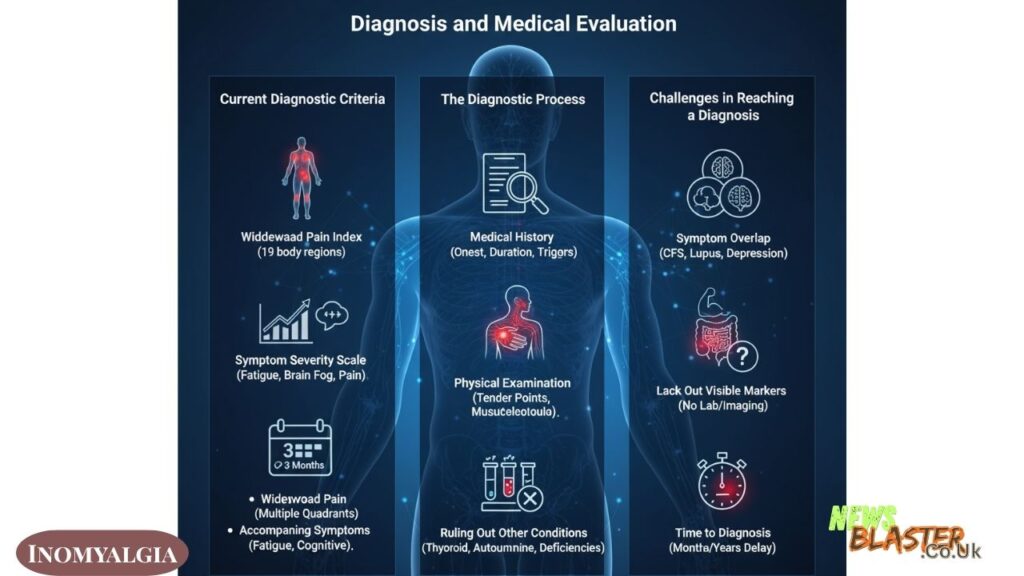
Current Diagnostic Criteria
Diagnosing this condition requires a comprehensive evaluation since no single laboratory test or imaging study can definitively confirm it. Healthcare providers rely on clinical assessment, symptom history, and ruling out other potential conditions. The diagnostic process can be lengthy and sometimes frustrating for patients seeking answers.
The Widespread Pain Index evaluates how many areas of the body experience pain. Patients indicate which of 19 designated body regions have been painful over the past week. This systematic assessment helps quantify the extent of pain distribution throughout the body.
The Symptom Severity Scale measures the intensity of key symptoms including fatigue, cognitive difficulties, and physical symptoms. Patients rate symptom severity on a numerical scale, providing healthcare providers with quantifiable data about symptom burden.
For diagnosis, patients typically must have experienced widespread pain for at least three months. The pain should affect multiple body quadrants and be accompanied by characteristic symptoms such as fatigue and cognitive difficulties. The persistence and pattern of symptoms help distinguish this condition from acute or localized pain problems.
The Diagnostic Process
Medical history forms the foundation of evaluation. Healthcare providers ask detailed questions about symptom onset, duration, intensity, and factors that worsen or improve symptoms. Information about previous medical conditions, injuries, family history, and lifestyle factors helps create a comprehensive picture.
Physical examination includes assessment of tender points and overall musculoskeletal health. Providers may apply gentle pressure to specific body locations to evaluate pain response. While older diagnostic criteria emphasized tender point examination, current approaches focus more broadly on widespread pain and associated symptoms.
Ruling out other conditions represents a crucial diagnostic step. Many conditions produce similar symptoms, including thyroid disorders, vitamin deficiencies, inflammatory arthritis, and other rheumatic diseases. Laboratory tests such as complete blood counts, inflammatory markers, and thyroid function tests help exclude alternative explanations for symptoms.
Challenges in Reaching a Diagnosis
Symptom overlap with numerous other conditions complicates diagnosis. Chronic fatigue syndrome, multiple sclerosis, lupus, and depression share many features with this disorder. Distinguishing between these conditions requires careful evaluation and sometimes multiple medical consultations.
The lack of visible or measurable markers frustrates both patients and healthcare providers. Unlike conditions that show clear abnormalities on blood tests or imaging studies, this disorder does not produce objective markers that can be measured in a laboratory. The absence of concrete diagnostic evidence sometimes leads to patients feeling dismissed or doubted.
Time to diagnosis varies considerably but often takes months or years. Patients may consult multiple healthcare providers before receiving an accurate diagnosis. This diagnostic delay can prolong suffering and delay the implementation of appropriate treatment strategies.
Treatment and Management Approaches
Medication Options
Pain relievers provide symptom management for many patients. Over-the-counter medications such as acetaminophen or ibuprofen may offer mild relief. For more severe pain, healthcare providers may prescribe stronger analgesics. However, pain medications alone rarely provide complete symptom control and work best as part of a comprehensive treatment plan.
Antidepressant medications serve multiple therapeutic purposes beyond mood improvement. Selective serotonin and norepinephrine reuptake inhibitors help modulate neurotransmitter levels, which can reduce pain signals and improve sleep quality. Tricyclic antidepressants, taken at lower doses than used for depression, may also help with pain and sleep disturbances.
Anti-seizure medications have shown effectiveness in treating nerve-related pain. These medications work by calming overactive nerve signals. Several medications in this class have received approval for treating chronic pain conditions and may reduce pain intensity and improve function.
Sleep aids may be prescribed to address persistent sleep problems. Improving sleep quality often leads to reduced fatigue and better pain management. However, long-term use of sleep medications requires careful monitoring due to potential dependence and side effects.
Non-Pharmacological Therapies
Physical therapy provides individualized exercise programs designed to improve strength, flexibility, and function without worsening symptoms. Therapists teach proper body mechanics, pacing strategies, and techniques for managing pain during activities. Gradual exercise progression helps rebuild tolerance for physical activity.
Cognitive behavioral therapy addresses the psychological aspects of living with chronic pain. This therapy helps patients develop coping strategies, modify unhelpful thought patterns, and improve emotional resilience. CBT has demonstrated effectiveness in reducing pain-related disability and improving quality of life.
Stress management techniques play a vital role in symptom control. Chronic stress exacerbates pain and fatigue, creating a cycle that perpetuates suffering. Learning and practicing stress reduction methods such as deep breathing, progressive muscle relaxation, and mindfulness meditation can break this cycle.
Acupuncture and massage therapy offer alternative approaches to pain relief. While responses vary among individuals, many patients report temporary symptom improvement following these treatments. When incorporated into a comprehensive treatment plan, these complementary therapies may enhance overall well-being.
Occupational therapy helps patients adapt daily activities to reduce pain and conserve energy. Occupational therapists assess home and work environments, recommending modifications and assistive devices that make tasks easier. Learning efficient ways to accomplish daily activities prevents symptom exacerbation.
Lifestyle Modifications
Sleep hygiene improvement represents a foundational element of management. Establishing consistent sleep and wake times, creating a comfortable sleep environment, limiting screen time before bed, and avoiding caffeine late in the day all promote better sleep quality. Since poor sleep worsens pain and fatigue, prioritizing sleep hygiene yields significant benefits.
Regular low-impact exercise, despite seeming counterintuitive when in pain, proves beneficial for most patients. Activities such as walking, swimming, gentle yoga, or tai chi improve physical function without excessive strain. Starting slowly and gradually increasing activity levels helps prevent symptom flares while building endurance.
Stress reduction practices deserve daily attention. Chronic pain itself creates stress, which then amplifies pain perception. Breaking this cycle requires consistent stress management efforts. Techniques such as meditation, journaling, spending time in nature, or engaging in enjoyable hobbies all contribute to stress reduction.
Dietary considerations may influence symptom severity for some individuals. While no specific diet cures the condition, some patients report improvement after eliminating certain foods or adopting anti-inflammatory eating patterns. Maintaining a balanced, nutritious diet supports overall health and provides the body with resources needed for healing and function.
Pacing activities and conserving energy prevents overexertion that leads to symptom flares. Learning to balance activity with rest, breaking tasks into smaller segments, and recognizing personal limits helps maintain function while avoiding crashes. Energy conservation strategies enable patients to accomplish more overall by preventing exhausting boom-and-bust cycles.
Complementary and Alternative Approaches
Yoga and tai chi combine gentle movement with mindfulness and breathing techniques. These practices improve flexibility, strength, and balance while promoting relaxation. Many patients find these mind-body practices particularly helpful for managing both physical and emotional symptoms.
Meditation and mindfulness practices train attention and awareness. Regular practice can alter pain perception, reduce stress reactivity, and improve emotional regulation. Mindfulness-based stress reduction programs specifically designed for chronic pain have shown positive outcomes in research studies.
Supplements may provide benefits, though patients should consult healthcare providers before starting any new supplements. Some individuals report improvement with magnesium, vitamin D, or other nutritional supplements. Ensuring adequate nutrition and correcting deficiencies supports overall health and may influence symptom severity.
Hydrotherapy, including warm baths or pool exercises, offers pain relief for many patients. The warmth relaxes tense muscles while water buoyancy reduces pressure on joints and tissues. Aquatic exercise programs provide effective workouts without the impact stress of land-based activities.
Living with Chronic Pain
Daily Life Management Strategies
Coping strategies develop through experience and experimentation. Each person discovers which approaches work best for their unique situation. Keeping a symptom diary helps identify triggers and patterns, enabling more effective symptom management. Tracking activities, pain levels, sleep quality, and stress levels reveals connections that inform better decision-making.
Work accommodations enable many individuals to maintain employment despite symptoms. Flexible scheduling, ergonomic workstation modifications, the option to work from home, and understanding supervisors can make continued employment possible. Open communication with employers about limitations and needs facilitates necessary accommodations.
Social support systems provide emotional sustenance during difficult times. Family, friends, support groups, and online communities offer understanding, encouragement, and practical assistance. Connecting with others who face similar challenges reduces feelings of isolation and provides validation.
Self-advocacy skills empower patients to participate actively in their healthcare. Learning about the condition, asking questions, expressing concerns, and collaborating with healthcare providers as partners leads to better outcomes. Patients who advocate for themselves often receive more appropriate care and feel more in control of their health journey.
Impact on Quality of Life
Physical limitations affect many aspects of daily living. Tasks that once felt easy may now require significant effort or modification. Hobbies, recreational activities, and social engagements may need adjustment to accommodate symptom fluctuations. Accepting limitations while maximizing remaining abilities requires ongoing adaptation.
Emotional and mental health challenges accompany the physical aspects of living with chronic pain. Grief over lost abilities, frustration with persistent symptoms, worry about the future, and social isolation all take emotional tolls. Acknowledging these emotional impacts and seeking appropriate support helps maintain psychological well-being.
Relationship and social impacts can strain connections with loved ones. Family members and friends may struggle to understand invisible symptoms or know how to offer support. Communication about needs, limitations, and feelings helps maintain relationship quality. Educating loved ones about the condition fosters empathy and appropriate support.
Financial considerations add stress to an already challenging situation. Medical expenses, potential lost income due to reduced work capacity, and costs of treatments accumulate. Planning for financial impacts and exploring available resources such as disability benefits or assistance programs helps manage economic stress.
Support and Resources
Support groups provide opportunities to connect with others facing similar challenges. Both in-person and online groups offer spaces to share experiences, exchange coping strategies, and provide mutual encouragement. Many patients find tremendous value in connecting with others who truly understand their struggles.
Patient advocacy organizations offer education, resources, and community. These organizations work to raise awareness, fund research, and improve care for individuals with chronic pain conditions. Connecting with advocacy groups provides access to current information and opportunities to contribute to larger efforts.
Educational resources help patients and families understand the condition better. Reliable websites, books, and materials from medical organizations provide evidence-based information. Education empowers patients to make informed decisions and communicate effectively with healthcare providers.
Healthcare team coordination ensures comprehensive, consistent care. When multiple providers are involved, ensuring they communicate and coordinate treatment approaches prevents conflicting recommendations and ensures all aspects of care are addressed. Designating a primary care provider to coordinate care often improves outcomes.
Current Research and Future Directions
Research continues to investigate the underlying mechanisms that cause chronic pain conditions. Scientists study brain imaging, genetic factors, immune system function, and nervous system changes to better understand what goes wrong in these disorders. Improved understanding of causes may lead to more targeted, effective treatments.
New treatment approaches under investigation include novel medications, neurostimulation techniques, and innovative behavioral interventions. Clinical trials test promising therapies to determine effectiveness and safety. Participation in research studies not only advances scientific knowledge but may also provide access to cutting-edge treatments.
Biomarker research seeks objective measures that could simplify diagnosis and track treatment response. Identifying blood tests, imaging findings, or other measurable markers would revolutionize diagnosis and enable more personalized treatment approaches. While no reliable biomarkers currently exist, research in this area continues actively.
Improved diagnostic tools may emerge from ongoing research. Developing more objective, standardized diagnostic methods would reduce time to diagnosis and ensure patients receive appropriate care more quickly. Advances in understanding pain processing mechanisms may reveal new diagnostic approaches.
Patient registries and long-term studies track large groups of patients over time. These studies provide valuable information about disease progression, treatment outcomes, and factors that influence symptom severity. Long-term data helps researchers and clinicians better understand the condition’s natural history and optimize management strategies.
Addressing Common Misconceptions
The harmful “it’s all in your head” myth dismisses very real physical suffering. While psychological factors influence pain perception, this does not mean pain is imaginary or less valid. Chronic pain involves complex interactions between physical, neurological, and psychological factors. Understanding pain as a legitimate medical condition rather than a character flaw or psychological weakness is essential.
Misunderstanding invisible illness creates additional burdens for patients. Because pain, fatigue, and other symptoms are not visible to observers, patients may face skepticism or accusations of exaggeration. The invisible nature of symptoms does not make them less real or less debilitating. Education about invisible illnesses helps create more understanding and supportive environments.
Confusion with other conditions sometimes leads to inappropriate treatment or delayed diagnosis. While symptom overlap exists among various chronic pain and fatigue conditions, accurate diagnosis matters for optimal treatment. Different conditions may require different management approaches, making precise diagnosis important.
Stigma and validation challenges affect many patients. Living with a condition that others cannot see and that lacks definitive diagnostic tests sometimes leads to feelings of not being believed or taken seriously. Healthcare providers, family members, and society at large benefit from education that validates patient experiences and recognizes chronic pain as a legitimate medical condition.
Conclusion
Understanding this complex chronic pain condition requires recognizing that it involves much more than simple muscle soreness. The widespread pain, profound fatigue, cognitive difficulties, and numerous other symptoms significantly impact every aspect of life. While diagnosis can be challenging and no cure currently exists, effective management is possible through comprehensive approaches.
The importance of a multifaceted care approach cannot be overstated. Combining appropriate medications, physical therapies, psychological support, lifestyle modifications, and self-management strategies provides the best outcomes. No single treatment works for everyone, requiring individualized plans developed through collaboration between patients and healthcare providers.
Hope for improved understanding and treatment exists. Research continues to uncover new information about underlying mechanisms and potential therapeutic targets. As scientific knowledge advances, diagnostic processes improve and treatment options expand. Each year brings new insights that enhance the ability to help patients manage symptoms and improve quality of life.
Empowerment through knowledge and self-management enables patients to take active roles in their health. Understanding the condition, recognizing triggers, developing coping strategies, and maintaining healthy lifestyle habits all contribute to better outcomes. While living with chronic pain presents significant challenges, many individuals successfully manage symptoms and maintain meaningful, fulfilling lives.
Also Read: Two Steeples Medical Centre Your Trusted Healthcare Partner in Wigston